Claude Syndrome: An Overview
Claude Syndrome is a rare neurological condition characterized by a combination of symptoms resulting from a stroke in the midbrain. It is named after Henri Charles Jules Claude, a French psychiatrist and neurologist who first described the condition in 1912.
What is Claude Syndrome?
Claude Syndrome is a type of brainstem stroke syndrome that affects the midbrain, specifically the dorsomedial aspect. The midbrain is a part of the brainstem that plays a crucial role in motor movement, auditory and visual processing, and control of eye movements. Claude Syndrome is caused by an infarction (stroke) in this region, leading to a variety of neurological symptoms.
How Did Claude Syndrome Get Its Name?
The syndrome is named after Henri Charles Jules Claude, who first described it in 1912. Claude was a French psychiatrist and neurologist who made significant contributions to the field of neurology. His work on this particular syndrome led to its naming in his honor.
Signs and Symptoms
The clinical presentation of Claude Syndrome includes a combination of the following symptoms:
- Ipsilateral Oculomotor Nerve Palsy: This results in drooping eyelid (ptosis), dilated pupil, and eye deviation downward and outward (hypotropia and exotropia).
- Contralateral Hemiparesis: Weakness or partial paralysis of the opposite side of the body.
- Contralateral Ataxia: Lack of muscle coordination affecting the opposite side of the body.
- Contralateral Hemiplegia: Paralysis of the lower face, tongue, and shoulder on the opposite side.
- Cerebellar Tremor: Also known as rubral tremor or intention tremor, which is a lack of coordination of a limb to move accurately to an intended position.
- Dissociated Horizontal Nystagmus: Rapid involuntary eye movement when the eye moves horizontally.
What artery is affected by Claude syndrome?
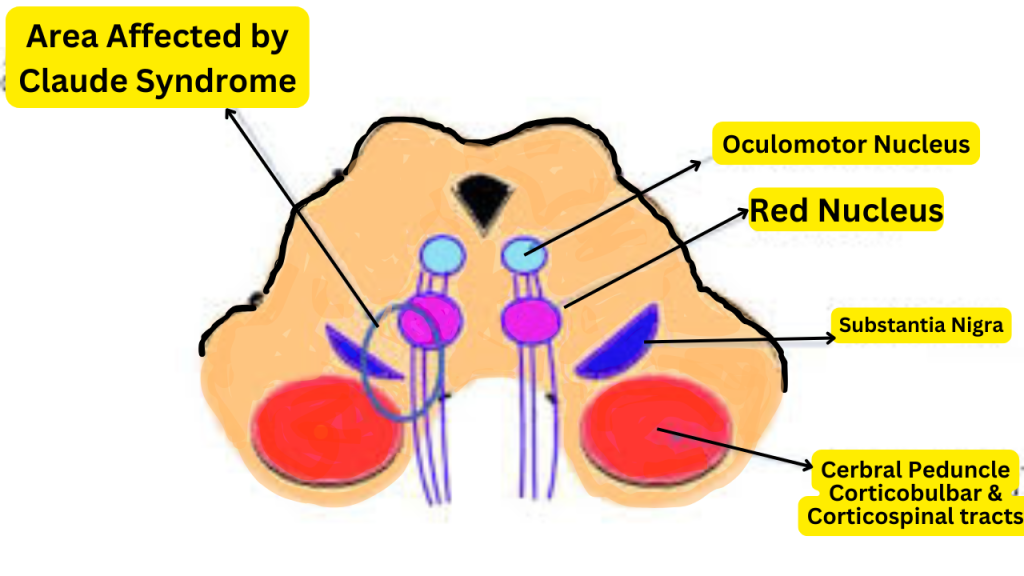
Claude Syndrome is typically caused by an occlusion of a small perforating branch of the posterior cerebral artery that supplies the dorsomedial aspect of the midbrain. This occlusion leads to ischemia (lack of blood flow) and subsequent infarction (tissue death) in the affected area.
Diagnostic Methods
Diagnosing Claude Syndrome involves a combination of clinical evaluation and imaging studies:
- Neurological Examination: Assessing the patient’s symptoms, including eye movement, muscle strength, coordination, and reflexes.
- Magnetic Resonance Imaging (MRI): Provides detailed images of the brain and can identify the location and extent of the infarction in the midbrain.
- Computed Tomography (CT) Scan: Can also be used to detect abnormalities in the brain, although MRI is more sensitive for this condition.
Treatment Options
Treatment for Claude Syndrome focuses on managing the underlying cause and alleviating symptoms:
- Anticoagulant Therapy: Medications to prevent further blood clots if the cause is related to a blood clotting disorder.
- Antiplatelet Therapy: Medications to prevent platelets from clumping together and forming clots.
- Rehabilitation: Physical therapy, occupational therapy, and speech therapy to help improve motor skills, coordination, and communication.
- Management of Risk Factors: Controlling high blood pressure, diabetes, and other conditions that increase the risk of stroke.
Complications
Potential complications of Claude Syndrome include:
- Permanent Neurological Deficits: Persistent weakness, coordination problems, and eye movement abnormalities.
- Increased Risk of Recurrent Stroke: Patients with Claude Syndrome are at a higher risk of experiencing another stroke.
- Psychological Impact: The condition can lead to emotional and psychological challenges due to the significant impact on daily functioning.
Risk Factors
Individuals at risk for Claude Syndrome include those with:
- Cerebrovascular Disease: Conditions that affect blood flow to the brain, such as atherosclerosis.
- Cardiovascular Disease: Conditions like atrial fibrillation that increase the risk of blood clots.
- Hypertension: High blood pressure can damage blood vessels and increase the risk of stroke.
- Diabetes: Poorly controlled diabetes can lead to complications that increase the risk of stroke.
Life Expectancy
The life expectancy of individuals with Claude Syndrome varies depending on the severity of the stroke, the effectiveness of treatment, and the presence of other medical conditions. Early diagnosis and management can improve outcomes and quality of life.
Difference Between Benedikt Vs Claude Syndrome
While both Claude Syndrome and Benedikt Syndrome are brainstem stroke syndromes, they have some differences:
- Claude Syndrome: Involves the dorsomedial midbrain, affecting the red nucleus, superior cerebellar peduncle, and oculomotor nerve.
- Benedikt Syndrome: Involves the ventral midbrain, affecting the red nucleus, corticospinal tract, and oculomotor nerve.
Both syndromes present with similar symptoms, such as oculomotor nerve palsy and contralateral hemiparesis, but the specific location and extent of the infarction differ.
References
- Claude HCJ. Les syndromes alternes du pédoncule cérébral (sémiologie, diagnostic, physiopathologie). Rev Neurol. 1912;20:202-210.
- Kumar A, Lalitha RM. Claude Syndrome. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK564370/
- Puccini K, Patel M, Murphy P. Claude’s Syndrome. Medscape. Updated Apr 2020.
- Brazis PW, Masdeu JC, Biller J. Localization in Clinical Neurology. 7th ed. Philadelphia: Wolters Kluwer Health; 2016.
- Bogousslavsky J, Fisher M. Textbook of Neurological Disorders. 2nd ed. Cambridge: Cambridge University Press; 2013.
FAQs about Claude Syndrome
1. What is Claude Syndrome, and what causes it?
Claude Syndrome is a rare neurological disorder stemming from a stroke in the midbrain’s dorsomedial area. This condition arises when there is an occlusion in a branch of the posterior cerebral artery, leading to restricted blood flow, ischemia, and eventual infarction in this region.
2. What are the primary symptoms of Claude Syndrome?
The main symptoms of Claude Syndrome include:
- Ipsilateral Oculomotor Nerve Palsy: Characterized by drooping eyelids, pupil dilation, and the eye deviating downward and outward.
- Contralateral Hemiparesis: Weakness or partial paralysis on the side of the body opposite the lesion.
- Contralateral Ataxia: Poor coordination on the opposite side.
- Cerebellar Tremor: Involuntary shaking, especially when trying to move a limb to a specific position.
3. How is Claude Syndrome diagnosed?
Diagnosis typically involves:
- Neurological Examination: To evaluate eye movement, muscle strength, and coordination.
- Imaging Techniques: MRI and CT scans help identify infarction and damage location in the midbrain.
4. What treatment options are available for Claude Syndrome?
Treatment focuses on managing the cause and alleviating symptoms:
- Medication: Anticoagulants and antiplatelet drugs to reduce the risk of further strokes.
- Rehabilitation: Physical, occupational, and sometimes speech therapy to improve coordination and motor skills.
- Risk Factor Management: Controlling blood pressure, diabetes, and other stroke risk factors.
5. How does Claude Syndrome differ from Benedikt Syndrome?
Though both are brainstem stroke syndromes, they affect different areas:
- Claude Syndrome: Affects the dorsomedial midbrain, leading to ipsilateral oculomotor nerve palsy, contralateral hemiparesis, and ataxia.
- Benedikt Syndrome: Involves the ventral midbrain and may cause oculomotor nerve palsy, contralateral hemiparesis, and, at times, tremors due to red nucleus involvement.
You May Also Like
How to Break Social Media Addiction in 2024: Proven Methods for Lasting Freedom
What is Phubbing? The Surprising Impact of This 2024 Relationship Killer
Hospital Information System: Don’t Miss Out on 2024 Healthcare Innovations