The anterior cruciate ligament (ACL) is one of the four major ligaments that stabilize the knee joint. It prevents excessive forward movement of the tibia (shin bone) on the femur (thigh bone) and limits rotational movements of the knee. The ACL can be injured by direct trauma, such as a collision or a fall, or by indirect mechanisms, such as twisting or pivoting. ACL injuries are common in sports that involve sudden changes of direction, such as soccer, basketball, and skiing.
One of the most reliable and sensitive tests to diagnose an ACL injury is the Lachman test. This test was developed by John Lachman, an orthopedic surgeon at Temple University in Philadelphia, in 1976. The Lachman test is performed by applying an anterior force on the tibia while stabilizing the femur with the knee flexed at about 20 to 30 degrees. The amount of anterior translation and the quality of the end-point are assessed and compared with the opposite knee.
Anatomy of the Knee Joint
Before we dive into the details of the Lachman Test, it’s important to understand the basic structure and function of the knee joint.
Structure and Function of the Knee Joint
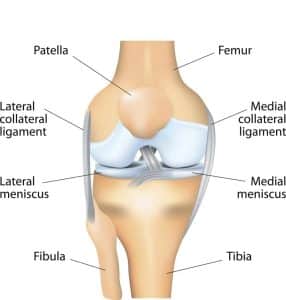
The knee joint is the largest joint in the body and is made up of three bones: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). The knee joint is responsible for bending and straightening the leg, as well as allowing rotation of the lower leg.
Components of the Knee Joint
The knee joint is also supported by a number of ligaments and muscles that work together to keep the joint stable. The ACL is one of the most important ligaments in the knee joint and is responsible for preventing the tibia from moving too far forward relative to the femur.
Anatomy and Physiology of the ACL
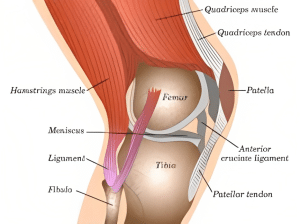
The primary function of the ACL is to control the anterior movement of the tibia and inhibit extreme ranges of tibial rotation. The ACL consists of 2 major bundles; the posterolateral bundle and the anteromedial bundle, which are named based on their tibial insertion. The bundles originate on the posteromedial side of the lateral femoral condyle and insert just anterior to the intercondylar tibial eminence. The Lachman test directly assesses the integrity of this anatomical relation.
(Read More About Fadir Test – How to Perform & Faber Test – Uses for Lower Back Pain)
What is the Lachman Test?
The Lachman Test is a physical examination technique used to assess the stability of the knee joint. It involves placing the knee in a certain position and then applying a gentle force to the lower leg bone (tibia) to see if there is any abnormal movement or “gapping” of the knee joint. If the test is positive, it may indicate a tear in the ACL.
Indications for Performing the Lachman Test
The clinician should ask about the timing of the injury, the mechanism, joint swelling, functional ability, joint instability, and associated injuries while performing an appropriate history and physical exam on a patient with a suspected ACL injury. Non-contact injuries most commonly cause ACL tears, and historical cues prompting an ACL evaluation include a sudden change of direction or awkward landing, causing the knee to “pop” or give way, resulting in knee pain, swelling, or instability.
Contraindications for Performing the Lachman Test
There are no absolute contraindications for performing the Lachman test. However, some factors that might affect its accuracy or feasibility include:
- Severe pain or swelling in the knee that makes it hard to bend at 20 to 30 degrees
- A torn meniscus that affects movement during the test
- A hamstring spasm that affects movement during the test
- The examiner’s hand size or position that prevents adequate stabilization or translation
- The patient’s lack of cooperation or consent
Technique and Grading of the Lachman Test
Preparation for the Lachman Test
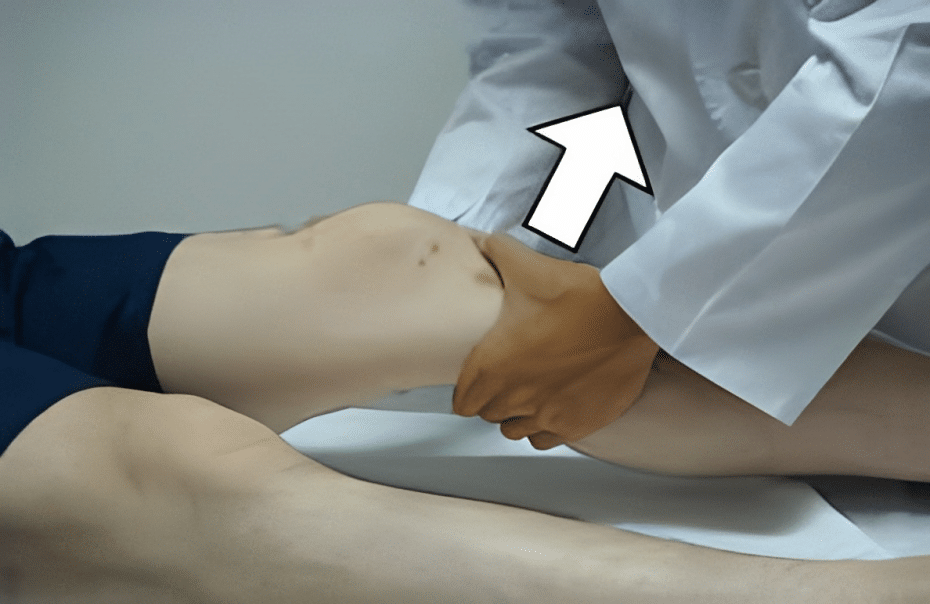
To perform the Lachman Test, the patient should lie down on their back with their knee bent at a 20-30 degree angle. The examiner will then sit on the patient’s foot to stabilize the leg.
Step-by-step guide on how to perform and grade the Lachman test:
- You lie down flat on your back, with your legs out straight and your muscles all relaxed, especially the hamstring muscles in your upper leg.
- Your doctor bends your knee slowly and gently to about a 20-degree angle. They may also rotate your leg so your knee points outward.
- Your doctor places one hand on your lower thigh and one hand on your lower leg just below where your leg bends. It is important that the examiner’s thumb be on the tibial tuberosity.
- Your doctor gently but firmly pulls your lower leg forward, keeping your thigh stable with the other hand.
- Your doctor observes and feels the amount of anterior translation and the quality of the end-point and compares them with the opposite knee.
- Your doctor grades your injury on this scale:
- Normal: No increased anterior translation or soft end-point compared with the opposite knee.
- Grade 1: Slight increase in anterior translation (2 to 5 mm) with a firm end-point.
- Grade 2: Moderate increase in anterior translation (5 to 10 mm) with a soft or mushy end-point.
- Grade 3: Marked increase in anterior translation (10 to 15 mm) with no discernible end-point.
Common Errors in Performing the Lachman Test
Common errors in performing the Lachman Test include not applying enough force, not stabilizing the leg properly, or not positioning the knee at the correct angle.
Accuracy and Limitations
Sensitivity: 85 – 94 %
Specificity: 91 – 99 %
Accuracy: 90 %
The Lachman test is considered to be one of the most accurate diagnostic tests for ACL injuries, with a reported accuracy rate of up to 90%. However, the Lachman test also has some limitations and challenges. The Lachman test requires skill and experience to perform accurately and consistently. It may be difficult to perform in patients with large thighs, muscular spasms, or guarding.
It may also miss partial ACL tears or combined injuries with other ligaments or menisci. It is particularly useful in the acute setting, but it should be used in conjunction with other diagnostic tools, such as MRI, to confirm the diagnosis. While the Lachman test is reliable, it may not detect all ACL injuries.
Comparison with Other Physical Examination Tests
The anterior drawer test, pivot shift test, and valgus stress test are other physical examination tests used to diagnose knee injuries, including ACL injuries. Compared to the Lachman test, the anterior drawer test has similar accuracy but is less reliable, while the pivot shift and valgus stress tests are more accurate but require a skilled examiner.
Clinical Significance and Implications of the Lachman Test
The Lachman test is a valuable tool for diagnosing ACL injury and guiding treatment decisions. It can help identify patients who may benefit from early surgical intervention or conservative management. It can also help monitor the progress and outcome of rehabilitation after ACL reconstruction. The Lachman test should be performed by trained clinicians who are familiar with its technique and interpretation.
Some of the clinical implications of the Lachman test are:
Positive Lachman Test
A positive Lachman test (grade 2 or 3) indicates a complete or near-complete ACL tear, which usually requires surgical repair to restore knee stability and function. Surgery should be considered within 3 weeks of injury to prevent further damage to the cartilage and menisci.
Negative Lachman Test
A negative Lachman test (normal or grade 1) indicates a partial or intact ACL, which may be managed conservatively with physical therapy, bracing, and activity modification. However, some patients may still experience instability or recurrent injuries, which may warrant surgical intervention.
False-Negative Lachman Test
A false-negative Lachman test may occur in patients with chronic ACL injuries, where scar tissue or secondary restraints may limit anterior translation.
False-Positive Lachman Test
A false-positive Lachman test may occur in patients with posterior cruciate ligament (PCL) injuries, where posterior sagging of the tibia may mimic anterior translation. Therefore, the Lachman test should be correlated with other clinical findings and imaging studies.
ACL Injury Management Strategies
Management strategies for ACL injuries depend on the severity of the injury, the patient’s age and activity level, and other factors. Treatment may include physical therapy, bracing, and surgery. The Lachman test can help healthcare providers decide on the appropriate management strategy for each patient.
Conclusion
The Lachman test is a simple, reliable, and sensitive test for diagnosing ACL injuries. It can help clinicians evaluate the integrity of the ACL, grade the severity of the injury, and plan the appropriate treatment. The Lachman test should be performed with proper technique and interpretation, and in conjunction with other tests and imaging studies when needed. The Lachman test can help improve the outcomes and quality of life of patients with ACL injuries.
You May Also Like
- Tips for Getting Better Sleep with Anxiety in 2024
- Split Renal Test: The Best Way to Diagnose Dangerous Kidney Problems in 2024
- Revolutionizing Treatment-Resistant Schizophrenia Solutions: Unleashing Hope in 2024
- Demystifying Obsessive-Compulsive Disorder in 2024: Understanding OCD from the Inside Out
- Unmasking the Mind: Can the DAP Test Truly Decode Your Mind in 2023?