Atheroma: What You Need to Know
Atheroma is a medical term that refers to the buildup of fatty material inside the arteries. This material, also known as plaque, is composed of cholesterol, calcium, inflammatory cells, and other substances that circulate in the blood. Atheroma can cause the arteries to narrow and harden, reducing the blood flow to the organs and tissues. This condition is called atherosclerosis and can lead to serious health problems such as heart attack, stroke, peripheral artery disease, and kidney failure.
Definition of Atheroma
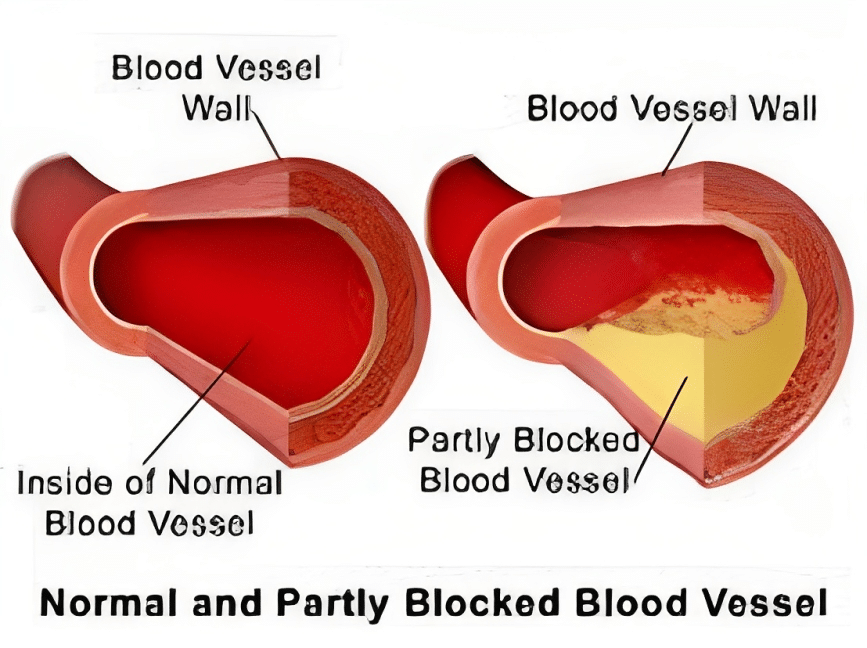
The word atheroma comes from the Greek words athērē, meaning paste, and oma, meaning tumor. However, atheroma is not a tumor or a cancer. It is a substance that accumulates in the inner layer of the arterial wall, called the endothelium. The endothelium is normally smooth and flexible, allowing the blood to flow freely. However, when the endothelium is damaged by factors such as high blood pressure, diabetes, smoking, or inflammation, it becomes inflamed and attracts white blood cells. These cells transform into foam cells that trap fat and cholesterol in the arterial wall. Over time, this process leads to the formation of atheroma.
Signs and Symptoms of Atheroma
The signs and symptoms of atheroma depend on which arteries are affected. If the coronary arteries are affected, you may experience symptoms of heart disease, such as:
- Chest pain (angina)
- Shortness of breath
- Fatigue
- Palpitations
- Dizziness
- Fainting
If the carotid or vertebral arteries are affected, you may experience symptoms of stroke, such as:
- Weakness or numbness in the face, arm, or leg, especially on one side of the body
- Sudden confusion, trouble speaking or understanding speech
- Sudden trouble seeing in one or both eyes
- Sudden trouble walking, maintaining balance, or coordination
- Sudden severe headache with no known cause
If the peripheral arteries are affected, you may experience symptoms of peripheral artery disease (PAD), such as:
- Leg pain when walking or exercising (claudication)
- Cold or numb feet
- Sores on the feet or toes that don’t heal
- Changes in the color of the skin on the feet or toes
Atheroma Grading
Atheroma grading is a way of measuring the severity of atherosclerosis in the arteries. There are different methods of grading atheroma, such as angiography, ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), or intravascular ultrasound (IVUS). These methods can provide information about the size, shape, location, and composition of the plaque. One common way of grading atheroma is by using the American Heart Association (AHA) classification system. This system divides atheroma into six types:
- Type I: Minimal changes in the endothelium with no visible plaque.
- Type II: Fatty streaks or spots in the endothelium with no significant narrowing of the artery.
- Type III: Intermediate lesions with small plaques that may slightly reduce the artery diameter.
- Type IV: Atheromatous core lesions with large plaques that may significantly reduce the artery diameter.
- Type V: Fibroatheroma lesions with thick fibrous caps covering the plaques.
- Type VI: Complicated lesions with ulcerated or ruptured plaques that may cause thrombosis or embolism.
Types of Atheroma
There are two main types of atheroma:
Stable atheroma: This type of plaque is stable and does not cause any symptoms. It is usually found during routine medical examinations or imaging tests.
Unstable atheroma: This type of plaque is unstable and can rupture or break off, causing a blood clot to form. This can lead to a stroke or TIA (transient ischemic attack).
Atheroma can also be classified based on its location in the body. Some common types of atheroma include:
- Skin atheroma: Also known as sebaceous cysts or epidermoid cysts, benign growths that form under the skin due to blocked sebaceous glands. They are not related to atherosclerosis and do not pose any serious health risk. They can be removed surgically if they cause discomfort or cosmetic problems.
- Carotid atheroma: These are plaques that form in the carotid arteries, which supply blood to the brain. They can cause transient ischemic attacks (TIAs) or strokes if they block or rupture the artery. Symptoms may include sudden weakness, numbness, vision loss, speech difficulty, or confusion. Carotid atheroma can be treated with medications, surgery, or endovascular procedures such as angioplasty or stenting.
- Aortic atheroma: These are plaques that form in the aorta, which is the largest artery in the body. They can cause chest pain, abdominal pain, back pain, leg pain, or claudication (pain while walking) if they reduce the blood flow to the heart or other organs. They can also cause aortic aneurysms (ballooning of the artery wall) or dissections (tearing of the artery wall) if they weaken or rupture the artery. Aortic atheroma can be treated with medications or surgery.
- Coronary atheroma: Plaque in the coronary arteries, which supply blood to the heart.
- Peripheral artery disease (PAD): Plaque in the arteries of the legs and feet.
Atheroma can also be classified based on its composition. Some common types of plaque include:
- Fatty streaks: The earliest form of atheroma, fatty streaks are small yellow deposits of fat on the inner lining of the artery.
- Fibrous plaques: These plaques are more advanced and contain more fibrous tissue.
- Calcified plaques: The most advanced type of plaque, calcified plaques contain calcium deposits.
The type of atheroma that a person has can affect their risk of complications. For example, an unstable atheroma is more likely to rupture and cause a stroke or TIA. Calcified plaques are also more likely to rupture, but they are less likely to cause a total blockage of the artery.
Risk Factors of Atheroma
Atheroma and atherosclerosis are common conditions that affect millions of people worldwide. They are influenced by both genetic and environmental factors. Some risk factors for developing atheroma are:
- Age: The risk of atherosclerosis increases with age as the arteries become less elastic and more prone to damage.
- Sex: Men and postmenopausal women are more likely to develop atherosclerosis than premenopausal women due to hormonal differences.
- Family history: Having relatives who have had heart disease or stroke at an early age increases the risk of inheriting genes that predispose to atherosclerosis.
- Smoking: Smoking damages the endothelium and increases inflammation and oxidative stress in the arteries. It also lowers HDL (good) cholesterol and raises LDL (bad) cholesterol levels in the blood.
- High blood pressure: High blood pressure puts extra strain on the arterial walls and causes them to thicken and stiffen. It also increases the risk of plaque rupture and thrombosis.
- High cholesterol: High cholesterol levels in the blood contribute to plaque formation in the arteries. LDL cholesterol is especially harmful as it can penetrate the endothelium and accumulate in the arterial wall. HDL cholesterol is beneficial as it can remove excess cholesterol from the arteries and transport it to the liver for excretion.
- Diabetes: Diabetes causes high blood sugar levels that damage the endothelium and increase inflammation and oxidative stress in the arteries. It also lowers HDL cholesterol and raises triglyceride (fat) levels in the blood.
- Obesity: Obesity is associated with increased levels of inflammation, oxidative stress, and insulin resistance in the body. It also raises blood pressure, cholesterol, and triglyceride levels in the blood.
- Physical inactivity: Physical inactivity reduces the blood flow and oxygen supply to the arteries. It also lowers HDL cholesterol and raises LDL cholesterol and triglyceride levels in the blood.
- Diet: A diet high in saturated fat, trans fat, cholesterol, salt, and sugar can increase the risk of atherosclerosis. A diet low in fiber, antioxidants, and omega-3 fatty acids can also hurt arterial health.
How to Prevent Atheroma Build-up
The prevention and management of atheroma and atherosclerosis involve lifestyle changes and medications. Some of the recommended lifestyle changes are:
- Quitting smoking: Quitting smoking can improve endothelial function and reduce inflammation and oxidative stress in the arteries. It can also lower blood pressure, cholesterol, and triglyceride levels in the blood.
- Controlling blood pressure: Controlling blood pressure can prevent or delay the progression of atherosclerosis. It can also reduce the risk of plaque rupture and thrombosis. Blood pressure can be controlled by reducing salt intake, losing weight, exercising regularly, managing stress, and taking antihypertensive medications if prescribed by a doctor.
- Lowering cholesterol: Lowering cholesterol can slow down or reverse the formation of plaque in the arteries. It can also reduce the risk of plaque rupture and thrombosis. Cholesterol can be lowered by reducing saturated fat, trans fat, and cholesterol intake, increasing fiber intake, exercising regularly, losing weight, and taking lipid-lowering medications such as statins if prescribed by a doctor.
- Managing diabetes: Managing diabetes can prevent or delay the damage to the endothelium and reduce inflammation and oxidative stress in the arteries. It can also lower blood pressure, cholesterol, and triglyceride levels in the blood. Diabetes can be managed by controlling blood sugar levels with diet, exercise, weight loss, and medications such as insulin or oral hypoglycemic agents if prescribed by a doctor.
- Maintaining a healthy weight: Maintaining a healthy weight can improve the blood flow and oxygen supply to the arteries. It can also lower blood pressure, cholesterol, triglycerides, inflammation, and oxidative stress levels in the body. A healthy weight can be achieved by balancing calorie intake with physical activity, following a balanced diet that includes fruits, vegetables, whole grains, lean proteins, low-fat dairy products, nuts, seeds, and healthy oils, and avoiding processed foods that are high in fat, salt, sugar, and additives.
- Increasing physical activity: Increasing physical activity can strengthen the heart muscle and improve its efficiency.
FAQs
What is Atheroma?
Atheroma is a buildup of fatty material inside the arteries. This can block blood flow to organs and tissues.
What are the symptoms of Atheroma?
Common symptoms include chest pain, shortness of breath, dizziness, and fainting.
What are the risk factors for Atheroma?
Risk factors include age, sex, family history, smoking, high blood pressure, high cholesterol, diabetes, obesity, and physical inactivity.
How is Atheroma diagnosed?
Atheroma can be diagnosed using imaging tests such as angiography, ultrasound, CT scan, and MRI.
How is Atheroma treated?
Treatment may include medications and/or surgery. Medications can lower blood pressure, cholesterol, and blood sugar levels, prevent blood clots, and reduce inflammation. Surgery can remove or bypass the plaque in the arteries or widen the artery with a balloon or a stent.
How can Atheroma be prevented?
Atheroma and atherosclerosis can be prevented or delayed by making lifestyle changes such as quitting smoking, controlling blood pressure, lowering cholesterol, managing diabetes, maintaining a healthy weight, increasing physical activity, and following a balanced diet.
You May Also Like
Extrapyramidal Symptoms Due to Haloperidol – Click Here
Clozapine Side Effects: Click Here
Flag Hair Sign in Kwashiorkor: Click Here